
Īlthough scleritis has been strongly associated with systemic inflammatory and infectious diseases, and one of its most common complications is corneal involvement, such as peripheral corneal thinning, stromal keratitis, and peripheral ulcerative keratitis (PUK), the association between necrotizing scleritis and TMD has never been reported. TMD typically presents as a unilaterally or asymmetrically bilateral peripheral corneal thinning, peripheral opacity with lipid deposition, corneal neovascularization, pseudopterygium formation, and astigmatism. Besides, Terrien’s Marginal Degeneration (TMD) is a quite rare disease that usually presents in men between 40 and 59 years of age. This disorder occurs more frequently in women older than 60 years and is frequently associated with systemic inflammatory diseases. Necrotizing anterior scleritis is divided into two forms, with inflammation or without inflammation (scleroma-lacia perforans). Scleritis is classified according to the anatomical site and characteristics of the inflammation in the anterior (diffuse, nodular, and necrotizing) and posterior (diffuse and nodular) segments of the eye.
Scleritis is a severe inflammatory condition characterized by edema and inflammatory cell infiltration of the sclera. Thus, scleritis was related to the adjacent inflammatory process associated with TMD, as an atypical presentation of this disease. The patient did not meet the criteria for any systemic illness associated with scleritis, such as autoimmune diseases or vasculitis. The patient was referred to the rheumatologist and started treatment with systemic corticosteroids and cyclophosphamide, exhibiting a clinical improvement. At the slit-lamp examination, necrotizing anterior scleritis with a high risk of perforation in OS was observed. Seven months later, she presented with severe pain, decreased visual acuity, and photophobia in OS. Years later, she attended the ocular immunology consultation for a second opinion where TMD with ocular inflammatory component OU was diagnosed. Initially, she was diagnosed with conjunctivitis and treated with topical antibiotics and corticosteroids, with mild transitory improvement but the progression of the disease.
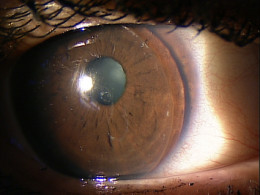
A 32-year-old female consulted for bilateral ocular burning and hyperemia.


 0 kommentar(er)
0 kommentar(er)
